|
Mains Exam
- General Studies Paper-1: Population and related issues, poverty and developmental issues.
- General Studies Paper-2: Topics related to development and management of social sector/services relating to health, education, human resources.
|
References
The Household Consumption Expenditure Survey (HCES-2022-23) data show a significant decline in poverty rates. However, it highlights the persistent vulnerability of the bottom 50 per cent of Indian households to the healthcare burden.
State of expenditure on health services
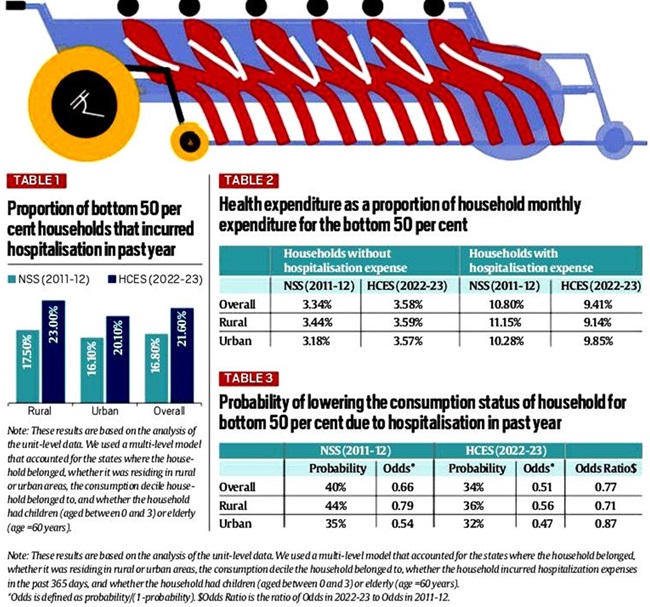
- Hospitalisation Expenditure: The proportion of the bottom 50% of households affording hospitalisation increased from 17% in 2011-12 to 22% in 2022-23.
- For rural households, this figure increased from 18% to 23%, and for urban households, it increased from 16% to 20%.
- Improved access to healthcare: This increase in healthcare expenditure reflects a significant improvement in access to healthcare for the poorest 50% of the population in both rural and urban areas of India.
- Health Expenditure Ratio: For the bottom 50% of households, health expenditure without hospitalisation increased marginally from 3.3% of monthly household expenditure in 2011-12 to 3.6% in 2022-23.
- In contrast, households with hospitalisation saw a significant decline in the share of health expenditure as a proportion of monthly household expenditure, falling from 10.8% to 9.4% over the same period.
- Economic burden: Health shocks deprive individuals of their independence, and the associated large medical expenses also place an economic burden on family members.
- Precious resources are diverted from other expenditure items to those needed to provide medical care.
Rural-urban gap in health expenditure ratio
- According to the Household Consumption Expenditure Survey (2022-23), healthcare with hospitalisation costs is becoming more affordable for the poorest 50% of the Indian population, especially in rural areas.
|
Rural area
|
- For the bottom 50%, the proportion of health expenditure without hospitalisation increased slightly from 3.4% to 3.6% over 11 years.
- For households that had hospitalisation, the proportion declined from 11.15% to 9.14% during the same period.
|
|
Urban Area
|
- The proportion of health expenditure for households that did not have to be hospitalised increased from 3.2% to 3.6%.
- For households that had to be hospitalised, the proportion decreased from 10.3% to 9.9%.
|
Economic impact on families of hospitalization
- Among the poorest 50%, 40% of households that were hospitalised in 2011-12 experienced a decline in consumption status.
- By 2022-23, despite an increase in the incidence of hospitalisation, only 33% of these households experienced a decline in consumption status.
- This effect is more pronounced in rural areas, where 44% of the bottom 50% of households that could afford hospitalisation faced a decline in consumption status in 2011-12, declining to 36% by 2022-23.
- For poor urban households, the probability of experiencing a decline in consumption status due to hospitalisation declined by 14% over 11 years.
Access and affordability of health services
- Recognizing the severe burden of medical expenses, the Government of India has implemented important policies to reduce this financial stress.
- Over the last decade, as a result of the government's health policies, healthcare has become more accessible and affordable for the bottom 50% of the Indian population.
- These trends are closely linked to public health initiatives in India, particularly the Ayushman Bharat scheme, which aims to reduce the financial burden of hospitalisation for the poor.
- Ayushman Bharat Yojana was launched as per the recommendation of National Health Policy 2017.
- The scheme aims to provide pioneering interventions to holistically address the health care system (covering prevention, promotion and ambulatory care) at the primary, secondary and tertiary levels.
- Ayushman Bharat follows a continuum of care approach, comprising two inter-related components –
- Health and Wellness Centres (HWCs)
- Pradhan Mantri Jan Arogya Yojana (PM-JAY)
- These initiatives help alleviate the immediate financial burden and reduce the risk of families falling into poverty due to health shocks.
The way forward
- Health Insurance Coverage: Programmes like the Ayushman Bharat Yojana should be strengthened and expanded to ensure comprehensive coverage and access to health insurance as a safeguard against rising health care costs.
- Improving access to primary health care: Primary health care is widely regarded as the most inclusive, equitable, and cost-effective way to achieve universal health coverage.
- Improving healthcare infrastructure and services in rural and urban areas under the National Health Mission (NHM) can enhance access to primary health care.
- Social determinants of health: Addressing social determinants such as education, sanitation and nutrition is important to reduce vulnerability to health shocks.
- Identifying these determinants and assessing community health needs to be accompanied by multi-sectoral policies to effectively address them.
- Preventive healthcare: Preventive healthcare can substantially reduce long-term healthcare costs. For example, regular vaccinations and screenings can prevent serious health problems, reducing the need for expensive treatments.
- Monitoring health expenditure trends: Health expenditure ratios and hospitalisation rates should be assessed regularly.
- This will help identify trends and areas requiring intervention and ensure timely responses to emerging challenges.
- Policy Impact Evaluation: Continuous evaluation of the effectiveness of health policies and programmes enables data-based adjustments to improve their impact on poverty reduction and health access.



